Source
HSCs are found in the bone marrow of adults, which includes femurs, hip, ribs, sternum, and other bones. Cells can be obtained directly by removal from the hip using a needle and syringe, or from the blood following pre-treatment with cytokines, such as G-CSF (granulocyte colony-stimulating factors), that induce cells to be released from the bone marrow compartment. Other sources for clinical and scientific use include umbilical cord blood, placenta, molilized peripheral blood. For experimental purposes, fetal liver, fetal spleen, and AGM (Aorta-gonad-mesonephros) of animals are also useful sources of HSCs.
Functional Characteristics
Multipotency and self-renewal
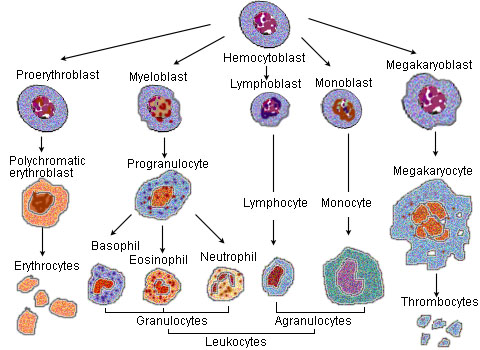
As stem cells, they are defined by their ability to form multiple cell types (multipotency) and their ability to self-renew.
It is known that a small number of HSCs can expand to generate a very large number of progeny HSCs. This phenomenon is used in bone marrow transplant when a small number of HSCs reconstitute the hematopoietic system. This indicates that, at least during bone marrow transplant, symmetrical cell divisions that give two progeny HSCs must occur, as expansion in HSC numbers seen during bone marrow transplant cannot occur in any other way.
Stem cell self-renewal is thought to occur in the stem cell niche in the bone marrow, and it is reasonable to assume that key signals present in this niche will be important in self-renewal. There is much interest in the environmental and molecular requirements for HSC self-renewal, as understanding the ability of HSC to replenish themselves will eventually allow the generation of expanded populations of HSC ex vivo that can be used therapeutically.
Lineage-Bias
Using limiting dilution strategies combined with other streamlined experimental and statistical methods for examining HSCs at the clonal level, it was shown that HSCs fall into three distinct lineage-bias[1] [2] [3] clusters. These are quantitatively defined by the ratio ρ of lymphoid to myeloid cells that HSC generate upon differentiation (which makes ρ a peripheral predictor for the clonal association of a reconstituted hematopoietic system). Balanced HSCs repopulate peripheral white blood cells in the same ratio of myeloid to lymphoid cells as seen in unmanipulated mice (on average about 15% myeloid and 85% lymphoid cells, or 3≤ρ≤10). Myeloid-biased (My-bi) HSC give rise to too few lymphocytes resulting in ratios 0 < ρ < 3, whereas lymphoid-biased (Ly-bi) HSC generate too few myeloid cells, which results in lymphoid-to-myeloid ratios of 10 < ρ < oo. All three types are normal HSC in that they have self-renewal capacity and can regenerate all hematopietic lineages (pluripotency). What is striking to note is that the lineage-bias is preserved through multiple rounds of serial transplantation: Balanced HSC self-renew to give rise to daughter HSC that are also balanced, My-bi HSC give rise to My-bi daughter HSC, and Ly-bi produce Ly-bi daughter HSC. There is no precursor-progeny relationship between the three types of HSC and they do not represent stages of differentiation. Rather, these are three classes of HSC, each with an epigenetically-fixed differentiation program.
Functional Assays
Cobble stone area-forming Cell (CAFC) assay: This is a cell culture based empirical assay. When plated onto a confluent culture of stromal feeder layer, a fraction of HSCs creep between the gaps (even though the stromal cells are touching each other) and eventually settle between the stromal cells and the substratum (here the dish surface) or trapped in the cellular processes between the stromal cells. Emperipolesis is the in vivo phenomenon in which one cell is completely engulfed into another (e.g., thymocytes into thymic nurse cells); on the other hand, when in vitro, lymphoid lineage cells creep beneath nurse-like cells, the process is called pseudoemperipolesis. This similar phenomeonon is more commonly known in HSC field by the cell culture terminology cobble stone area-forming cells (CAFC), which means areas of cluster of cells that look dull cobblestone-like under phase contrast microscopy, compared to the other HSCs, which are refractile. This happens because the cells that are floating loosely on top of the stromal cells are spherical and thus refractile. However, the cells that creep beneath the stromal cells are flattened and thus not refractile. The mechanism of pseudoemperipolesis is only recently coming to light. It may be mediated by interaction through CXCR4 (CD184) the receptor for CXC Chemokines (e.g., SDF1) and α4β1 integrins.[4].
Mobility
HSCs have a higher potential than other immature blood cells to pass the bone marrow barrier, and thus may travel in the blood from the bone marrow in one bone to another bone. If they settle in the thymus they'll develop into T cells. In the case of fetuses and other extramedullary hematopoiesis HSCs may also settle in the liver or spleen and develop.
This ability is the reason why HSCs may be harvested directly from the blood.
end first part.... from www.wikipedia.org
Nessun commento:
Posta un commento